By Charles A. Pilcher MD FACEP
September, 2013
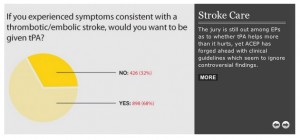
I am often asked to evaluate the medical records of stroke patients, almost always to address the issue of whether or not the provision of tPA, the “clot-busting drug,” would have provided a patient with a demonstrably better chance of an improved outcome following a stroke.
There remains considerable debate on the value of tPA in the treatment of stroke. While it has become the standard of care in treating stroke cases (for patients who qualify), the numbers are less than impressive when it comes to assessing actual overall benefit. The benefit is clearly marginal. No study has shown an absolute chance of improvement in excess of 50%. Without going into a complete review of all available studies, studies generally show that patients treated with tPA seem to have a better outcome compared to “no treatment” in from 5% to at most 15% of cases.
A recently published ACEP policy is surprisingly ambivalent on the issue, using the words “offered” and “considered” rather than the more powerful word “administered.” One is led to conclude that, while tPA may benefit some patients, the data is underwhelming that it benefits most.
This forces both patients, physicians, and attorneys, both defense and plaintiff, to view the issue cautiously. I have covered this issue in more detail below for those who are interested, and included further references at the end.
First, a quick review of “relative” and “absolute” benefit.
“Relative” benefit means the amount of benefit provided to a group of treated patients compared to the results in a group of untreated patients. Example: With treatment A, 4% of patients survive. Without treatment, 3% of patients survive. 4% is 1/3 better than 3%, so the “relative” benefit is 1/3, or 33%.
“Absolute” benefit means the amount of benefit from the treatment in absolute terms, e.g., in the example above, the difference between 4% and 3% is 1%. So, 1% is the “absolute” benefit of treatment A.
I discussed this concept in a previous “Perspective,” and used the following analogy: Suppose my chance of winning the lottery is one in a million. Suppose I develop a system that improves my chances of winning the lottery to one in 100,000. Do I now have a 90% better chance of winning the lottery? Yes. Do I now have a 90% chance of winning the lottery? No. My chance of winning increased from 0.000001 to 0.00001, or only 0.000099. The former number is my “relative” increased chance of winning. The number 0.000099 is my “absolute” increased chance of winning the lottery.
Even using “relative” benefit instead of “absolute” benefit, there is only about a 34% chance that the treated patient will do better.
“Loss of chance”
So, in states where “loss of chance” or “loss of opportunity” is applicable, it probably does not matter how great the benefit of a treatment might be. So long as there is any potential benefit to a treatment, failure to offer that treatment may be an arguable issue.
But in other states where one must be able to show that a treatment could have benefited a patient on a “more probable than not” basis, tPA consistently falls short. In fact, data show that never does the benefit of treatment exceed the 50% threshold that allows one to say that the patient would have improved on a “more probable than not” basis.
ACEP’s clinical policy on tPA in stroke
In February, 2013, the American College of Emergency Physicians (ACEP) published its policy statement on the use of tPA in stroke. The policy resulted from the work of an ACEP Study Group using the following methodology:
- 1140 potentially useful articles on the subject were identified, of which 303 were selected for further review and grading for strength of evidence.
- These articles were then sorted into 3 classes of evidence based on the design of the study, with design 1 representing the strongest evidence and design 3 representing the weakest.
- Articles were then graded on an additional 6 dimensions such as blindedness, bias, generlizability, sample size, etc.
- A final grade was assigned (Class I, II or III), with Class I being the strongest.
- Clinical findings and strength of recommendations regarding patient management were then made based on the quality of the evidence. ACEP applied the following criteria in evaluating the evidence:
- Level A recommendations. Generally accepted principles for patient management that reflect a high degree of clinical certainty (ie, based on strength of evidence Class I or overwhelming evidence from strength of evidence Class II studies that directly address all of the issues).
- Level B recommendations. Recommendations for patient management that may identify a particular strategy or range of management strategies that reflect moderate clinical certainty (ie, based on strength of evidence Class II studies that directly address the issue, decision analysis that directly addresses the issue, or strong consensus of strength of evidence Class III studies).
- Level C recommendations. Other strategies for patient management that are based on Class III studies, or in the absence of any adequate, published literature, based on panel consensus.
ACEP policy recommendations
The Study Group then produced ACEP’s “Patient Management Recommendations” in the published report “Clinical Policy: Use of Intravenous tPA for the Management of Acute Ischemic Stroke in the Emergency Department.” Below are excerpts:
-
- Level A recommendations. In order to improve functional outcomes, IV tPA should be offered to acute ischemic stroke patients who meet National Institute of Neurological Disorders and Stroke (NINDS) inclusion/exclusion criteria and can be treated within 3 hours after symptom onset. (The key word here is “offered.”)
- Level B recommendations. In order to improve functional outcomes, IV tPA should be considered in acute ischemic stroke patients who meet European Cooperative Acute Stroke Study (ECASS) III inclusion/exclusion criteria and can be treated between 3 to 4.5 hours after symptom onset. (The key word here is “considered.”)
- “Footnotes” to the above were included:
-
- The effectiveness of tPA has been less well established in institutions without the systems in place to safely administer the medication.
- Within any time window, once the decision is made to administer IV tPA, the patient should be treated as rapidly as possible.
- As of this writing, tPA for acute ischemic stroke in the 3- to 4.5-hour window is not FDA approved.
-
Conclusion
One should note the apparent ambivalence in the use of the words “offered” and “considered” in the statements above. These are certainly less powerful verbs than “administered.” One is led to conclude that, while tPA may benefit some patients, the data is underwhelming that it benefits most. This forces both patients, physicians, and attorneys to view the issue cautiously.
Further reading for both defense and plaintiff attorneys:
-
- ACEP News, April, 2013. Scroll to page 20 for a superb “Point/Counterpoint” debate regarding the new ACEP Clinical Guideline.
- In Emergency Physicians Monthly, May 29, 2013, Kevin Klauer MD discusses “indication creep,” the phenomenon whereby the use of a marginally effective therapy is expanded to new or broader indications. One could argue that the expansion of tPA to the treatment of stroke – after being proven reasonably effective in the treatment of coronary thrombosis – is itself an example of “indication creep.” Another would be the recommendation that it be used for the “wake up stroke,” when “last seen normal” time is undetermined. Dr. Klauer also addresses the issue of informed consent, which is necessary whenever the patient is offered the option of tPA, and whether or not the patient is treated with it.
- Stroke. 1992;23:641-645. In this original 1992 uncontrolled study of the safety of tPA for stroke, one finds this comment:“The rate of early neurological improvement observed in this study was small but does not exclude an improvement over the natural history.” This appears to be a less than enthusiastic endorsement.
- Emergency Physicians Monthly, July 8, 2013. Here, Dr. David Newman argues that thrombolytic therapy for stroke has a long way to go to be proven effective. He discusses the “Number Needed to Treat (NNT)” before a therapeutic benefit can be shown, and does so with simple graphics.
- Emergency Physicians Monthly editor Dr. Mark Plaster summarized the issue
- AAEM Position Statement: The Use of Intravenous Thrombolytic Therapy in the Treatment of Stroke, March, 2007. This includes an elegantly simple graphic on page 2 demonstrating the role that tPA may play in the treatment of stroke. In summary, were there 2 groups of 18 stroke patients each, one group receiving placebo and one group receiving tPA, the results would be as follows:
-
-
- 6 patients in each group will do poorly,
- 9 patients in each group will do well,
- only 3 of either group of 18 patients will have their outcome modified by tPA, and of those 2 will be helped and 1 will be harmed.
- Thus, the number needed to treat (NNT) for 1 patient to improve is 9, i.e., you have an 11% chance of receiving benefit from tPA, and
- the number needed to harm (NNH) is 18, i.e., you have a 4.5% chance of being made worse by tPA. And, finally,
- the actual degree of benefit for the two patients out of 18 who might be helped is variable, with no guarantees of complete recovery.
-